| Yeon-Hwan Park | 2 Articles |
Purpose
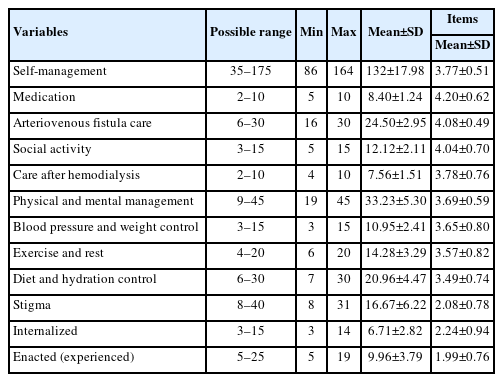
This study aimed to examine the relationship between stigma and self-management among patients undergoing hemodialysis and to identify the key factors influencing their self-management practices. Methods: A convenience sample of 139 hemodialysis patients, aged 18 years or older with an arteriovenous fistula, was recruited from online websites designed for patients undergoing hemodialysis in South Korea. Data were collected using a self-reported questionnaire that assessed demographic and clinical characteristics, self-management behavior, and stigma. Data analysis included descriptive statistics, the independent t-test, one-way analysis of variance, Pearson r correlations, and hierarchical regression analysis to evaluate the influence of stigma on self-management. Results: Hierarchical regression analysis showed that demographic and clinical characteristics accounted for 25.1% of the variance in self-management, and the inclusion of stigma increased the explained variance to 31.4%. Significant predictors included the number of hemodialysis sessions per week (≥3) (β=–.38, p<.001), stigma (β=–.27, p<.001), monthly household income (≥4 million won) (β=.24, p=.014), and marital status (single) (β=–.18, p=.028). Conclusion: The findings highlight the substantial impact of stigma and treatment burden on self-management, while socioeconomic status and marital support serve as protective factors. Targeted interventions that reduce stigma and strengthen support systems are warranted.
Purpose
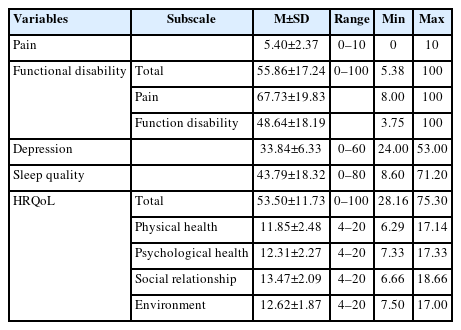
This study investigated health-related quality of life (HRQoL) and aimed to identify factors influencing HRQoL for patients with rotator cuff tears (RCTs). Methods: We conducted a descriptive correlational survey with 118 outpatients diagnosed with RCTs at a tertiary general hospital in Seoul. Data were collected between February and June 2021 using structured self-report questionnaires, including the numeric rating scale, Korean version of the Shoulder Pain and Disability Index, Verran and Snyder-Halpern Sleep Scale, and the World Health Organization Quality of Life Instrument, Short Form. Results: HRQoL showed significant positive correlations with sleep quality (r=.64, p<.001) and the frequency of shoulder-intensive sports activities (r=.24, p=.008). It was negatively correlated with symptom days per week (r=–.32, p<.001), symptom hours per day (r=–.51, p<.001), pain (r=–.21, p=.025), functional disability (r=–.49, p<.001), and depression (r=–.60, p<.001). Stepwise regression analysis indicated that sleep quality (β=.36, p<.001) was the strongest predictor of HRQoL, followed by occupation (β=.26, p<.001), depression (β=–.24, p=.010), and symptom hours per day (β=–.19, p=.013). Conclusion: Sleep quality was the most influential factor affecting HRQoL in patients with RCTs. These findings underscore the need for comprehensive nursing interventions that address sleep disturbances, provide psychological support for depressive symptoms, consider occupational demands, and promote early management of prolonged symptoms to enhance HRQoL in this population.
|
|